- 光半導体関連
ウェアラブル血糖モニタリングの進化──CGMの最新技術とデクセリアルズの貢献
【免責事項】
本記事の内容は、一般的な技術情報および市場動向の紹介を目的としたものであり、特定の医療行為・治療方法・診断・処方を推奨するものではありません。
記載されている情報は、医療従事者または医療機器関連事業者向けの参考資料として提供しています。一般消費者による医療判断や使用目的での参考はご遠慮ください。
本記事に記載された製品・材料・技術については、必ずしも医療機器として薬機法上の認可を受けているものではありません。実際の使用にあたっては、各国・地域の法規制および承認状況をご確認ください。
また、記事内容は執筆時点の情報に基づいており、将来的に変更される可能性があります。
目次
はじめに:より手軽で高精度な血糖管理を目指して
血糖値のモニタリングは、糖尿病患者にとって欠かせない日常管理の一部です。近年では、非侵襲かつ連続的に血糖をモニタリングできるウェアラブルデバイスの実用化が進んでおり、患者のQOL向上や医療負担の軽減が期待されています。
なぜ血糖モニタリングが重要なのか
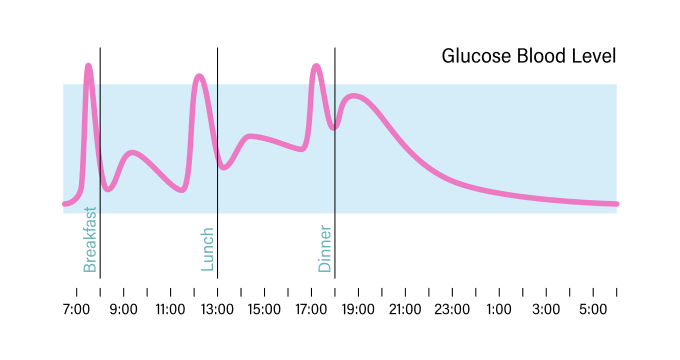
血糖値の管理は、糖尿病患者だけでなく、健康意識の高い人々にとっても重要な健康指標のひとつです。血糖値は食事や運動などの影響を受けて変動し、通常は食前で70~100mg/dL、食後でも140mg/dL未満が望ましいとされています。
特に1型・2型糖尿病患者にとっては、インスリン投与・食事・運動・生活習慣のバランス管理が不可欠であり、精度の高い血糖モニタリングが治療方針を左右する重要な要素となります。
連続血糖モニタリング(CGM)とは?
従来の自己血糖測定(SMBG)は、指先に針を刺して血液を採取し、その場で血糖値を測定する方法でした。近年はデバイスの小型化が進んだものの、1日に複数回の採血が必要で、患者の身体的・心理的負担は依然として大きいのが実情です。
一方でCGMでは、皮膚に装着した電極を通じて、間質液中のグルコース濃度をリアルタイムかつ連続的に測定します。装着したまま最大2週間のモニタリングが可能で、SMBGでは把握できなかった日中の血糖変動や夜間の低血糖リスクなども把握できます。
さらに、最近のCGMデバイスはアプリと連携し、スマートフォンでの遠隔モニタリングやアラート通知も可能になっています。
CGMは以下のような方に適しています:
- 1型または2型糖尿病の方
- 頻繁にインスリンを使用している方
- 低血糖リスクが高い方、または症状に気づきにくい方
- 血糖変動が大きい方
- 血糖データの共有が治療に有効な方
このようにCGMは、患者と医療従事者の両者にとって有益な情報を提供し、治療の最適化を支援するツールとなっています。

技術革新と市場動向:人工膵臓の登場と多様なセンサ技術
CGMとインスリンポンプを連携させた「クローズドループシステム(人工膵臓)」の開発が進んでおり、すでにアメリカや日本の1型糖尿病患者で導入が始まっています。
英国ケンブリッジ大学の研究では、人工膵臓が2型糖尿病患者にも有効であることが示され、血糖値の目標範囲内の時間が2倍、高血糖時間が半減するなどの効果が報告されました。こうしたシステムは、患者の負担を最小限に抑えつつ、血糖値の変動に応じて自動的にインスリン量を調整することで、日々の自己管理の手間を軽減します。さらに近年は、従来の電気化学式センサだけでなく、光学式や赤外線方式など、新たな非侵襲型センサの開発も進んでおり、市場の選択肢は拡大を続けています。

拡大する糖尿病人口と医療課題
国際糖尿病連合(IDF)によると、2021年時点で世界の糖尿病人口は5億3,700万人、成人の約10人に1人に相当します。この数字は2045年には7億8,300万人にまで増加すると見込まれており、特に低・中所得国での急増が顕著です。世界保健機関(WHO)は、糖尿病が2030年までに死因の第7位になると予測しており、医療費や生産性損失を含めた社会的・経済的負担も深刻化しています。加えて、新型コロナウイルス感染症の流行によって、血糖管理の不備が感染症の重症化リスクを高めることも明らかとなり、日常的な血糖管理の重要性が再認識されています。
デクセリアルズが貢献できること:CGMを支える材料技術
CGMの普及と高性能化を支える上で、デバイスの小型化・高信頼性接続・非侵襲性が重要なテーマとなっています。
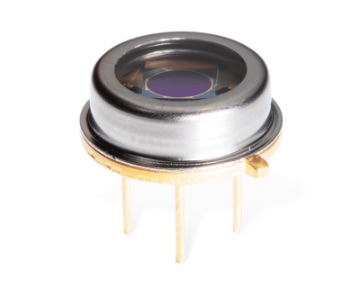
デクセリアルズの異方性導電膜(ACF)は、CGMの表示ディスプレイ部や内部回路との接続に広く用いられており、小型化と高密度実装の両立を実現しています。米国では保険適用の要件として装着型モニタが必須となっており、患者が常時携帯する機器へACFは大きく貢献しています。また、侵襲型センサ基板においても、はんだやメカニカルコネクタを不要とするACF接続技術により、センサ構造の小型・軽量化が進められています。加えて、赤外線方式の非侵襲型グルコースセンサの研究開発が進む中で、デクセリアルズの連結子会社であるデクセリアルズ フォトニクス ソリューションズ社のフォトダイオードも、将来的に光検出素子としての活用が期待されています。
デクセリアルズグループは、医療やヘルスケア分野をはじめとするさまざまなデバイスの小型化と性能向上に引き続き取り組んでおり、CGMをはじめとする技術の進歩に今後も貢献していきます。
関連記事
- SHARE
当社の製品や製造技術に関する資料をご用意しています。
無料でお気軽にダウンロードいただけます。
お役立ち資料のダウンロードはこちら
当社の製品や製造技術に関する資料をご用意しています。
無料でお気軽にダウンロードいただけます。
お役立ち資料のダウンロードはこちら